Nurse Care Planning in Schools
The National Association of School Nurses (NASN) School Nursing Practice Framework™ has four principles, Community/Public Health, Leadership, Quality Improvement and Care Coordination. The principle of care coordination encompasses the competencies of developing and implementing plans of care, providing direct care to students, and collaboration with families, health care providers and the entire school community. This is a framework for chronic condition management by nurses for students.
The American Academy of Pediatrics (AAP) in cooperation with a broad group of health, including NASN, and education agencies released in 2021 a Consensus Statement on the Core Tenets of Chronic Condition Management in Schools. The purpose of this framework of 7 core tenets and 3 foundational supports is drawn from the Chronic Care Model, NASN School Nursing Practice Framework™ and CDC Whole School, Whole Community, Whole Child, and others is to promote and optimize both health and educational outcomes.
Providing health and education equity demands that schools address the chronic health condition of student to promote and optimize health and academic outcomes for ALL students. Student learning cannot be separated from student health, they are intertwined.
Nurses by education, licensure and clinical experience are the subject matter experts in the school for chronic health condition management. Health Services Staffing explains in detail the legal scope of nursing practice for License Practical Nurses (LPN) and Registered Nurses (RN). RNs include Licensed School Nurses (LSN) and Public Health Nurses (PHN). While all nurses have a valuable role and contribute to care planning, only the RN can independently develop the care plan as defined in the Minnesota Nurse Practice Act. As defined in the Nurse Practice Act, LPNs participate with other health care providers in the development of care plans.
The National Association of School Nurses (NASN) which is the professional nursing organization for the specialty practice of school nursing, with the approval of ANA developed the School Nursing Scope and Standards of Practice, 4th Edition (2022). The Standards of Practice outlines the 6 standards of the nursing process that all RNs practicing in school nursing are expected to show competence.
- Standard 1: Assessment
- Standard 2: Diagnosis
- Standard 3: Outcomes Identification
- Standard 4: Planning
- Standard 5: Implementation
- Standard 5A: Coordination of Care
- Standard 5B: Health Teaching and Health Promotion
- Standard 6: Evaluation
It is through the nursing process how a RN/LSN/PHN determines the needs of students, identifies the intended outcome of care, develops the plan to meet needs and attain outcomes and then evaluates the effectiveness of that plan of care.
In the specialty practice of school nursing the RN/LSN/PHN most often develops an Individual Health Plan (IHP) and/or an Emergency Care Plan (ECP) to meet student health needs. These plans or components of these plans are also used within special education for an Individual Educational Plan (IEP) or for students who quality for accommodations through Section 504 to meet student health needs.
IHPs are nursing care plans written by RN/LSN/PHN using the nursing process in nursing language to guide care provided by nurses or those who provide care delegated/or assigned by the RN/LSN/PHN. The NASN has a robust position statement Use of Individualized Healthcare Plans to Support School Health Services.
An IHP serves multiple purposes:
- Maintain health status to optimize learning.
- Safe school and learning environment.
- Maintain, increase participation in the learning environment.
- Meet the daily health needs of students.
- Respond appropriately for any emergency health needs.
- Foster self-care and independence as age and developmentally appropriate.
The RN/LSN uses critical thinking and nursing judgement to determine and prioritize which students should have an IHP. The IHP combines health needs into one document, helping to organize so consistent care is provided to the student. Needs may include education, medications, and treatments, and/or social and emotional care. While the nurse writes the IHP, it is important to receive parent/guardian and student input as they may help direct some of the goals for the plan.
The IHP may include a student’s emergency care plan and if may be referenced or included in a student’s 504 accommodation plan or Individual Education Plan.
Resources
SN Chat - School Nurse Chronic Health Assessment Tool is a resource to help nurses assess and develop an IHP. It includes templates for the following conditions: seizure, diabetes, sickle cell disease, life threatening allergies and asthma.
MDH has developed an Individualize Healthcare Plan template. The LSN/LSN will need to use professional judgment and the nursing process to tailor this template to be student specific. The template may need to be adjusted to align with individual school procedures/policy and school information system/electronic health record.
In the school setting, the ECP/EAP is developed and written by the RN/LSN/PHN or are received from a health care provider such as an Asthma Action Plan, Seizure Action Plan, Anaphylaxis Action Plan, or part of the Diabetic Management Plan. When a plan is written by the health care provider, the nurse is responsible for reviewing and clarifying any questions.
The ECP/EAP is needed students with known health conditions that are likely to result in a medical emergency, requiring immediate medication or treatment to prevent significant harm. All ECP/EAPs should written in lay language so that school staff member could respond appropriately. The ECP/EAP is a step-by-step direction ‘if you see this, do this’.
If the nurse receives an ECP/EAP from the health care provider, it most likely is not necessary for the nurse to create an additional plan. However, the nurse may write need to write an addendum or additional ECP/EAP if school setting specific information is needed to provide a safe and immediate response to the student’s health condition.
The nurse is the communicator and educator of the plan to school staff who are responsible to understand the student’s need and respond appropriately. The RN can use the ECP/EAP as part of the education and training under nursing delegation as appropriate.
It is important communicate this plan to staff need to know about the health condition and potential for a medical emergency so staff are prepared to act quickly if an emergency should occur. The school nurse, along with administration, need to determine how to alert school staff of individual student’s health conditions and ECP/EAPs.
Under Family Education Right to Privacy Act (FERPA), it is allowable to share student information for those with legitimate educational interest. It is NOT recommended to create a list with all students and their health conditions and hand out to staff. This practice may violate FERPA as there may be some staff that do not have a legitimate educational interest for some of the students on the ‘list’. Rather, utilizing electronic student record and some type of ‘alert’ or ‘flag’ indicating a student has a health condition is better practice. Then the teacher or staff member can follow up with the nurse to find out more information about the health condition.
The ECP/EAP may be referenced or included in a student’s 504 accommodation plan or Individual Education Plan.
Under Section 504, FAPE consists of the provision of regular or special education and related aids and services designed to meet the student's individual educational needs as adequately as the needs of nondisabled students are met.
Section 504 team members varies according to student needs and district process. The nurse has knowledge of both health and education and can serve as the bridge to describe how a major life activity is impacted and inform the school team. The nurse can assist with developing accommodations to meet the student’s need for the classroom and plan for the health accommodations delivered through school health services. The nurse may reference or integrated an IHP and/or ECP/EAP into the 504 plans.
The U.S. Department of Education provides fact sheets about section 504 protections for students with specific conditions.
Section 504 Protections for Students with Asthma
Section 504 Protections for Students with Diabetes
Section 504 Protections for Students with Epilepsy
Section 504 Protections for Students with Food Allergies
Section 504 Protections for Students with GER or GERD
Section 504 Protections for Students with Sickle Cell Disease
Students who receive special education services have an IEP which outlines the unique needs of the student and the specialized goals and objectives to help the student make educational progress.
Through the evaluation process school nursing may be identified as a necessary and related service for the student to meet their educational goals. The LSN interprets and synthesizes health related information to determine the impact to learning and the school environment. Then based on the evaluation, when the student has a health need that impacts learning and requires nursing services, the nursing services are documented on the IEP. The IHP or ECP/EAP may be referenced or included in a student’s IEP.
Minnesota Department of Education Special Education
Transition Planning
Healthcare transition planning is important for students with healthcare needs especially when transitioning from pediatric to adult healthcare. NASN Transition Planning for Students with Healthcare Needs position statement describes the vital role of the nurse to provide expertise, leadership, and care coordination for students. MDH Transitioning to Adult Health Care webpage provides additional information and resources to assist the nurse.
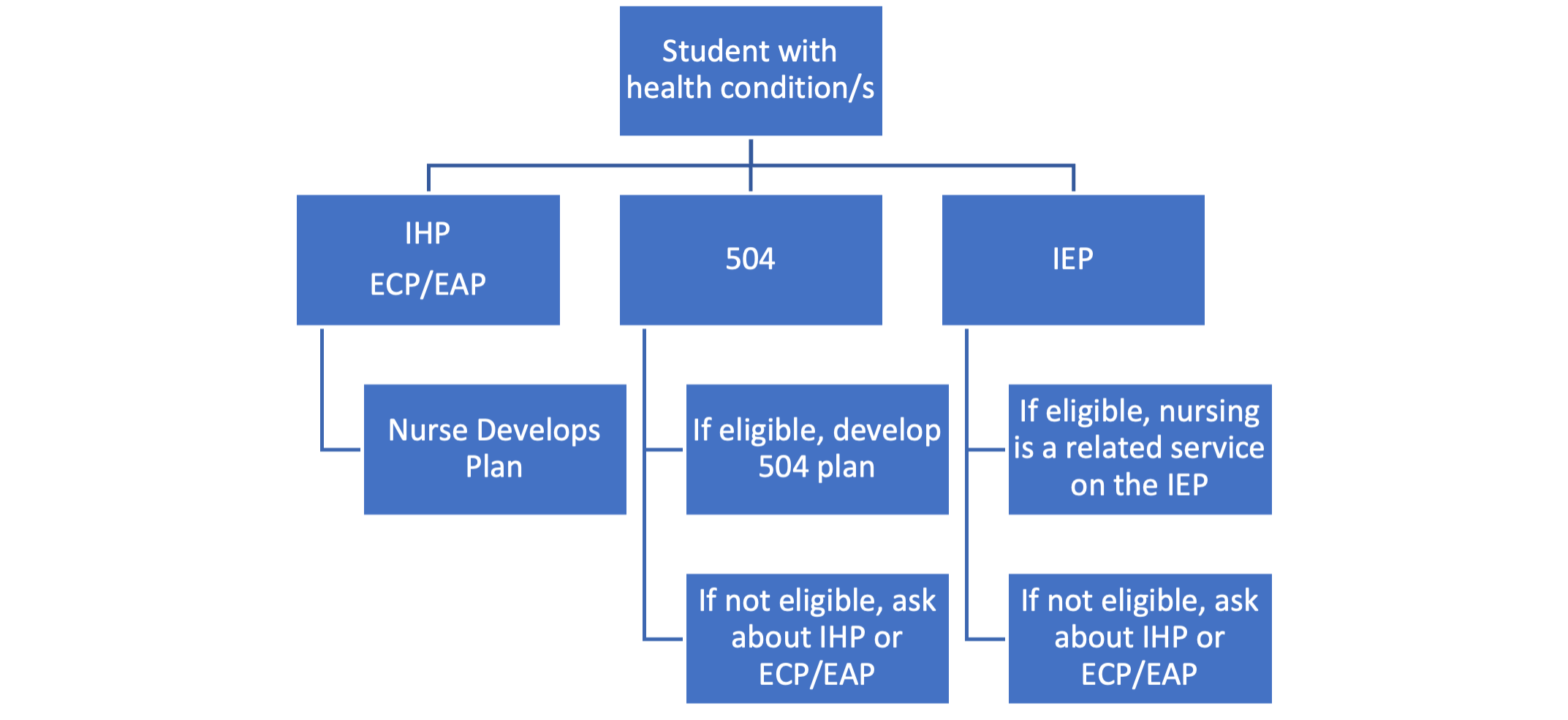
This graphic is meant to be a summary of the various types of care planning in school nursing practice as described above.